Oral Hygiene and Brain Health: Exploring the Relationship with Alzheimer’s Disease
Oral health and Alzheimer’s disease may seem unrelated at first glance, but emerging research over the past few years has begun to uncover intriguing connections between the health of our mouth and the health of our brain, specifically in the context of Alzheimer’s disease, a progressive neurological disorder that leads to memory loss and cognitive decline. This article delves into the current understanding of how oral health is related to Alzheimer’s disease, including the mechanisms behind this connection, the role of oral bacteria, and the implications for prevention and treatment strategies.

The Connection between Oral Health and Alzheimer’s Disease
The link between oral health and Alzheimer’s disease is primarily focused on inflammation and the presence of certain bacteria in the mouth that can potentially affect brain health.
Inflammation
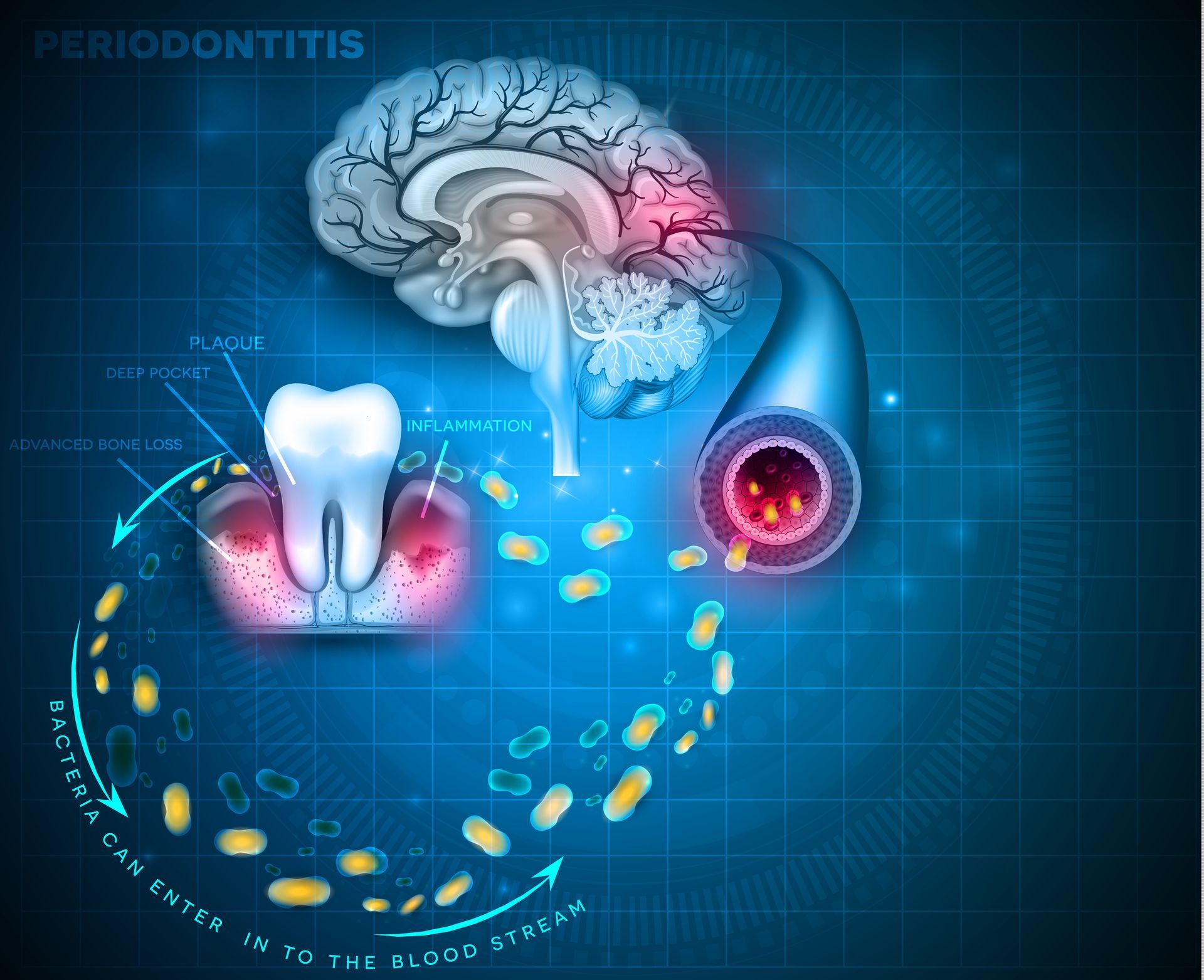
Chronic inflammation is a hallmark of poor oral health, often resulting from conditions such as gingivitis and periodontitis (advanced gum disease). This inflammation doesn’t stay localized to the mouth; it can enter the bloodstream and spread to other parts of the body, including the brain. Inflammation in the brain is a recognized factor in the development and progression of Alzheimer’s disease, suggesting a pathway through which poor oral health might contribute to the disease.
Oral Bacteria
Certain types of bacteria found in the mouth, particularly those associated with gum disease, such as Porphyromonas gingivalis, have been found in the brains of Alzheimer’s patients. P. gingivalis is known to produce a toxic enzyme called gingipains, which has been found in the neurons of Alzheimer’s patients. This presence of oral bacteria in the brain can lead to a direct form of neuroinflammation, potentially contributing to the development and progression of Alzheimer’s disease.
Evidence Linking Oral Health and Alzheimer’s Disease
Several studies have provided evidence supporting the connection between oral health and Alzheimer’s. For instance, research has found higher levels of oral bacteria in the brains of Alzheimer’s patients compared to those without the disease. Moreover, longitudinal studies have suggested that individuals with periodontitis have a higher risk of developing Alzheimer’s disease later in life compared to those with healthy gums.
Mechanisms Behind the Connection
The mechanisms behind the oral health-Alzheimer’s connection are still being unraveled but include:
• Direct Invasion of Pathogens: Bacteria from the mouth can enter the bloodstream through gum sores and make their way to the brain, potentially crossing the blood-brain barrier and causing inflammation directly within the brain tissue.
• Inflammatory Response: The systemic inflammation resulting from chronic oral infections can exacerbate inflammation in the brain, contributing to the pathology of Alzheimer’s.
• Immune System Activation: The chronic presence of oral bacteria can lead to a prolonged immune response, which, when misdirected, can attack healthy neurons, contributing to cognitive decline.
Implications for Prevention and Treatment
Understanding the connection between oral health and Alzheimer’s disease opens new avenues for prevention and treatment. Maintaining good oral hygiene practices—regular brushing, flossing, and dental check-ups—could potentially lower the risk of developing Alzheimer’s disease. It also highlights the importance of managing chronic oral infections not just for overall health but possibly as a preventive strategy against neurodegenerative diseases.
Furthermore, this connection presents potential therapeutic targets. For example, treatments aimed at reducing the burden of specific oral pathogens or modulating the inflammatory response might have implications for preventing or slowing the progression of Alzheimer’s disease.
Conclusion
The relationship between oral health and Alzheimer’s disease underscores the interconnectivity of our body’s systems and the importance of holistic health approaches. As research continues to evolve, it is becoming increasingly clear that maintaining oral health is not only vital for preventing dental problems but may also be crucial in protecting against more severe, systemic conditions, including Alzheimer’s disease. This connection emphasizes the importance of comprehensive health strategies that include the care of our mouth as a fundamental aspect of preventing and managing chronic diseases.